Alcoholic hepatitis is a liver disease that develops as a result of excessive and prolonged alcohol consumption.
Alcoholic hepatitis affects both men and women, regardless of their age.
What is an alcoholic liver disease?
Alcoholic hepatitis is an inflammation of the liver caused by excessive and prolonged alcohol consumption. “This is an acute pathology unlike alcoholic cirrhosis which is a chronic disease. In the case of cirrhosis, which can also be linked to heavy and prolonged alcohol consumption, the liver becomes fibrotic and hard.“, explains Dr Sarah Shili, gastroenterologist and hepatologist. People with alcoholic cirrhosis are also at greater risk of developing alcoholic hepatitis if they continue their alcohol consumption. We are talking about excessive consumption:
- In women: more than 40 grams of alcohol per day for the previous six months (1 glass of alcohol is equivalent to 10g of alcohol)
- In men: more than 60 grams of alcohol per day for the previous six months.
What are the symptoms of alcoholic hepatitis?
Symptoms of alcoholic hepatitis can vary depending on the severity of the disease and possible complications.
- Fatigue is one of the most common symptoms of alcoholic hepatitis. Due to liver dysfunction, the body may have difficulty metabolizing nutrients, which can lead to feeling constantly tired, including drowsiness.
- Jaundice (yellowing of the skin and eyes):it is due to an accumulation of bilirubin, a substance produced when red blood cells break down, due to liver dysfunction“, specifies our interlocutor.
- Sometimes, a distaste for alcohol leads the patient to withdraw spontaneously.
► The diagnosis of alcoholic hepatitis is based on a clinical-biological evaluation. Concretely, “The doctor begins by taking the patient’s history, including history of alcohol consumption and associated symptoms. It asks about the amount and duration of alcohol consumption, symptoms, and other medical history.”
► Blood tests are then carried out: they will measure in particular the levels of bilirubin, liver enzymes and prothrombin. These tests can reveal signs of inflammation and liver dysfunction. In acute alcoholic hepatitis, we classically find a moderate elevation of AST (aspartate aminotransferase) and ALT (alanine aminotransferase) with an AST/ALT ratio > 2 and a bilirubin > 100 µmol /L.
► A liver biopsy may be performed to confirm the diagnosis and assess the severity of inflammation and liver fibrosis. However, biopsy is not always necessary, particularly when the clinico-biological picture is typical.
Tool to evaluate the prognosis: Lille score, Maddrey score
The Lille and Maddrey scores are two tools commonly used after diagnosis to assess the severity of alcoholic hepatitis and guide treatment decisions.
► The Maddrey score is used to assess the severity of acute alcoholic hepatitis, underlines the specialist. It is based on blood parameters including prothrombin level and bilirubin concentration. A Maddrey score greater than 32 is often used as a cutoff to identify patients with severe acute alcoholic hepatitis. A high score suggests increased disease severity and may influence treatment decisions, such as the use of corticosteroids.
► The Lille score is used to assess treatment response in patients with acute alcoholic hepatitis who have been treated with corticosteroids. “It is calculated at the start of treatment and after one week of treatment. It incorporates parameters such as patient age, serum bilirubin and prothrombin level“, she continues. A high score at the end of the first week of treatment indicates an inadequate response and suggests a higher risk of death.
If the treatment does not work, it is stopped and a liver transplant may be considered.
The first step in treating alcoholic hepatitis is complete cessation of alcohol consumption, which is essential to prevent further liver damage. “First-line treatment involves taking corticosteroids, such as prednisolone, to reduce inflammation in the liver. The intake is 40 mg/day for 7 days.explains Dr Shili. After 7 days, the Lille score allows you to see if the patient responds favorably to the treatment. “If the treatment works (which is the case in around 75% of patients), it is continued for 1 month. It will be supplemented by addiction treatment and nutritional support. If it doesn’t work, we stop it.”. In this case, a liver transplant may be considered. This involves replacing the damaged liver with a healthy liver from a donor. But the transplant lists are extremely long. Access to transplantation in this context is highly regulated and requires a multidisciplinary assessment and a compliant patient who was previously unaware of their disease.
What life expectancy?
The life expectancy of a person with alcoholic hepatitis depends on several factors, including the severity of the disease, response to treatment, stopping alcohol use, the presence of complications, and medical management. “If treatment with corticosteroids works, the patient regains the life expectancy he had before alcoholic hepatitis. On the other hand, if the treatment does not work, there is a risk of death at 6 months in 75% of cases,” concludes the doctor.
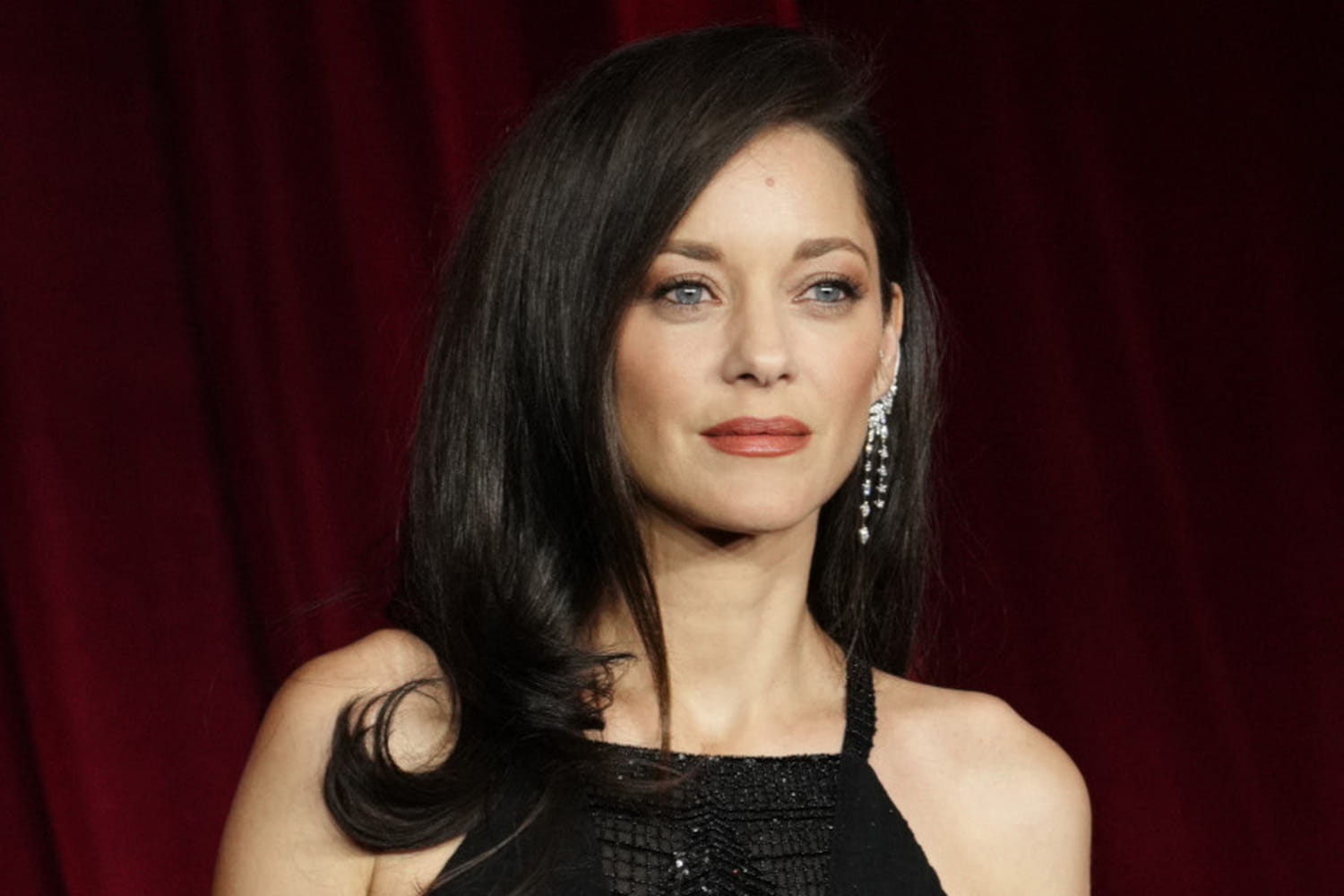
Thanks to Dr Sarah Shili, gastroenterologist and hepatologist, at the Polyclinique Bordeaux Nord (33).